Biden’s DOJ implies Obamacare harmed vital healthcare competition
The Antitrust Investigation Against UnitedHealth
A recent Wall Street Journal story has shed light on a new antitrust investigation targeting the largest health insurer in the United States. This investigation is just another example of the ongoing battle against the negative consequences of Obamacare, a law that has led to consolidation within the health sector.
Back in 2008, then-candidate Obama promised that his health care plan would reduce premiums by an average of $2,500 per family. However, the continuous rise in premiums demonstrates the failure of Obamacare according to Obama’s own standards. The law has also fostered anti-competitive behavior, which further explains the current situation.
Insurer’s Acquisition of Physician Groups
The Justice Department’s antitrust division is currently investigating the relationship between UnitedHealthcare’s insurance business and its subsidiary, Optum, which owns multiple physician practices. The investigation focuses on whether UnitedHealthcare has favored Optum-owned groups in its contracting practices, potentially excluding rival physicians from attractive payment arrangements. It also explores the impact of Optum’s ownership of health care providers on rival health insurers and compliance with federal rules regarding premium collection.
The new Justice Department inquiry … is partly examining Optum’s acquisitions of doctor groups and how the ownership of physician and health plan units affects competition. … Investigators have asked whether UnitedHealthcare favored Optum-owned groups in its contracting practices, potentially squeezing rival physicians out of certain types of attractive payment arrangements.
Investigators have also explored whether Optum’s ownership of health care providers could present challenges to health insurers that are rivals to UnitedHealthcare. … And investigators have asked whether and how the tie-up between UnitedHealthcare and Optum medical groups might affect its compliance with federal rules that cap how much a health insurance company retains from the premiums it collects from insurers.
Last year, Senator Elizabeth Warren and Senator Mike Braun requested an investigation into the evasion of medical loss ratio requirements by insurers through vertical integration. The Justice Department is now addressing this issue as well.
A Familiar Pattern
All of these issues are interconnected. Warren and Braun’s letter last year highlighted the impact of UnitedHealth’s insurance business and Optum’s physician practices. They also discussed the integration between pharmacies and pharmaceutical benefit managers (PBMs) who handle drug claims for insurance companies.
Similarly, hospitals have been engaging in mergers and acquisitions over the past decade, just like UnitedHealth’s acquisition of physician practices. A previous Wall Street Journal story from 2018 revealed how hospital mergers surged after the enactment of Obamacare in 2010.
These mergers have resulted in anti-competitive provisions that hinder transparency for employers and consumers. Even Walmart, known for its ability to negotiate lower prices, struggled to obtain a list of underperforming providers in its network due to these provisions.
The Impact of Obamacare
Obamacare has transformed much of the health care industry into regulated utilities, leading to mergers and acquisitions as companies seek to gain leverage through size. With profit percentages capped by regulations, these companies can only increase profits by expanding their revenue base.
Democrats are well aware of these issues. Warren’s letter acknowledged that companies like UnitedHealth were exploiting loopholes in the law, conveniently ignoring the fact that Democrats themselves created both the law and the loopholes.
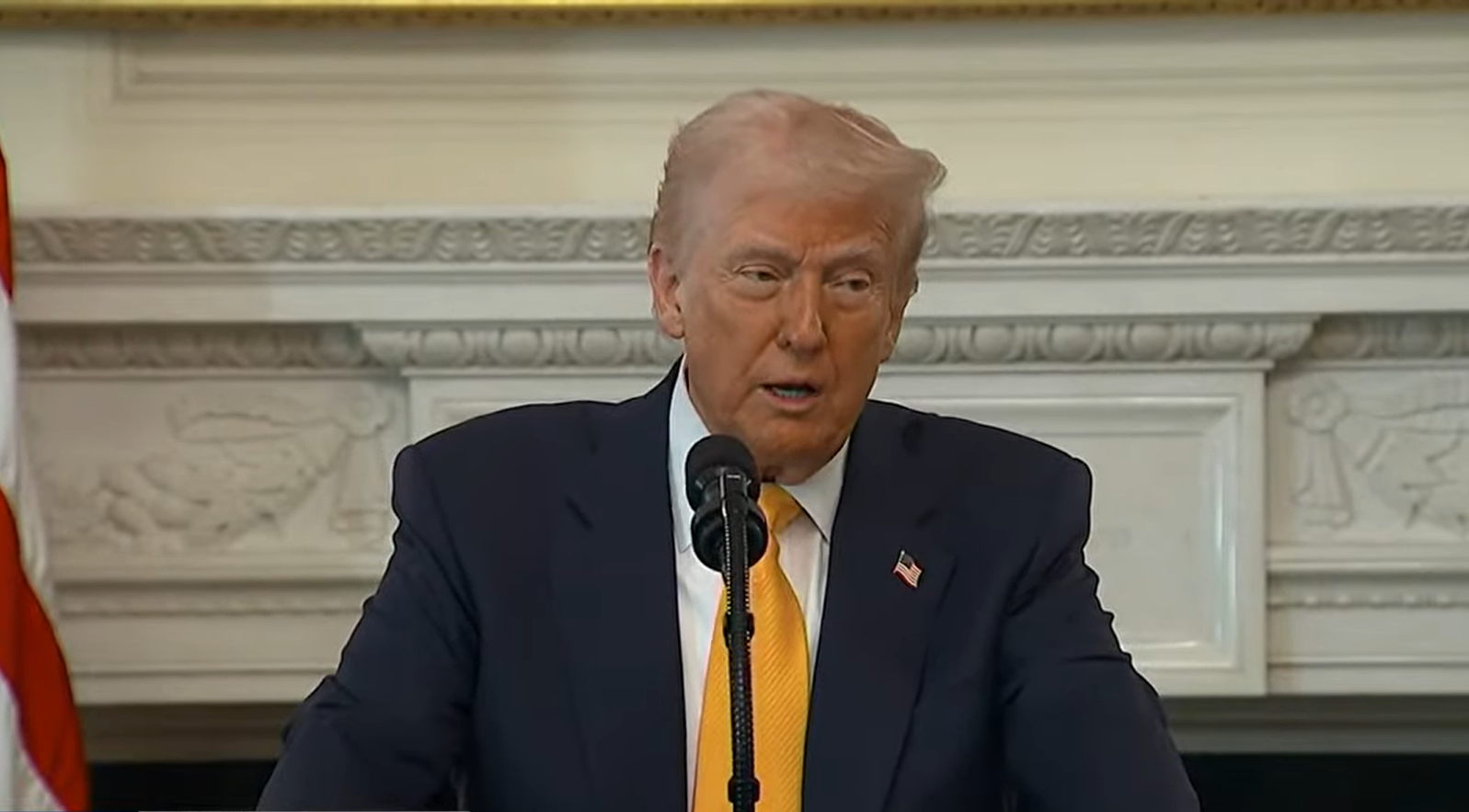
Warren unintentionally revealed the truth by referencing a blog post titled “How Obamacare Created Big Medicine.” This perfectly summarizes why, as President Trump stated, “Obamacare sucks.” The ongoing investigation by the Justice Department into UnitedHealth is an implicit admission of this fact, even under the Biden administration.
How are investigations into UnitedHealth’s relationship with Optum and the evasion of medical loss ratio requirements addressing the issues of consolidation, anti-competitive behavior, and compliance with federal rules within the healthcare industry
The recent antitrust investigation targeting UnitedHealth, the largest health insurer in the United States, has brought attention to the ongoing battle against the negative consequences of Obamacare. This investigation is just another example of how consolidation within the health sector has been fostered by the law.
Back in 2008, then-candidate Obama promised that his health care plan would reduce premiums by an average of $2,500 per family. However, the continuous rise in premiums demonstrates the failure of Obamacare according to Obama’s own standards. Furthermore, the law has also led to anti-competitive behavior within the industry, which further exacerbates the current situation.
The Justice Department’s antitrust division is currently investigating the relationship between UnitedHealthcare’s insurance business and its subsidiary, Optum, which owns multiple physician practices. The investigation focuses on whether UnitedHealthcare has favored Optum-owned groups in its contracting practices, potentially excluding rival physicians from attractive payment arrangements. It also explores the impact of Optum’s ownership of healthcare providers on rival health insurers and compliance with federal rules regarding premium collection.
The investigation is partly examining Optum’s acquisitions of doctor groups and how the ownership of physician and health plan units affects competition. Investigators have raised concerns about UnitedHealthcare favoring Optum-owned groups in its contracting practices, potentially squeezing out rival physicians from certain types of attractive payment arrangements. They have also explored whether Optum’s ownership of healthcare providers presents challenges to health insurers that are rivals to UnitedHealthcare. Investigators are also examining how the tie-up between UnitedHealthcare and Optum medical groups might impact its compliance with federal rules.
Last year, Senator Elizabeth Warren and Senator Mike Braun requested an investigation into the evasion of medical loss ratio requirements by insurers through vertical integration. The Justice Department is now addressing this issue as well.
All of these issues are interconnected. Warren and Braun’s letter last year highlighted the impact of UnitedHealth’s insurance business and Optum’s physician practices. They also discussed the integration between pharmacies and pharmaceutical benefit managers (PBMs) who handle drug claims for insurance companies.
Similarly, hospitals have been engaging in mergers and acquisitions over the past decade, similar to UnitedHealth’s acquisition of physician practices. A previous Wall Street Journal story from 2018 revealed how hospital mergers surged after the enactment of Obamacare in 2010.
These investigations and discussions shed light on the ongoing challenges within the healthcare industry. As the battle against the negative consequences of Obamacare continues, it is crucial to address the issues of consolidation, anti-competitive behavior, and compliance with federal rules. Only through a comprehensive understanding and resolve can a more efficient and fair healthcare system be achieved.
" Conservative News Daily does not always share or support the views and opinions expressed here; they are just those of the writer."




Now loading...