How to Fight “Immunity Aging”: Data Shows 9 out of 10 COVID Deaths Are Older Adults
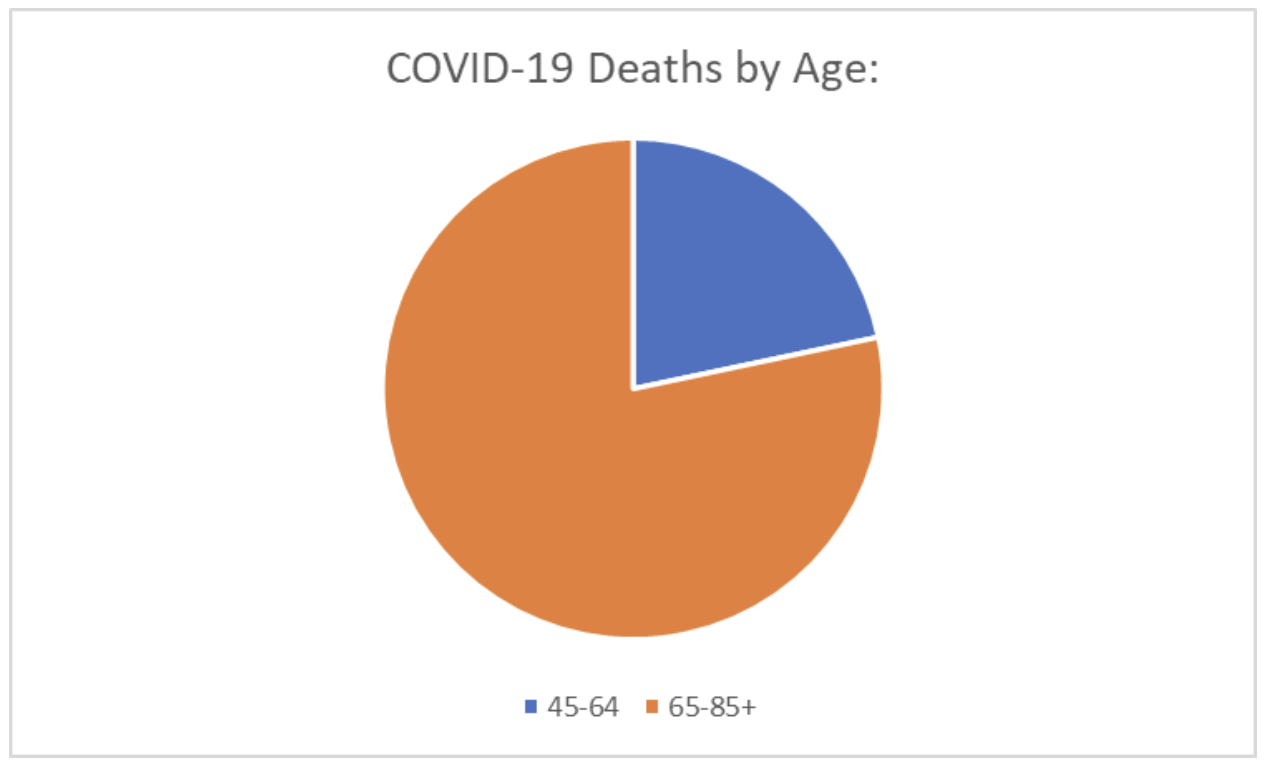
Analysis of COVID death data from the Centers for Disease Control and Prevention (CDC) in recent weeks found nearly 9 in 10 COVID deaths are reported among the 65 and older age demographic. As of the week ending Dec. 3, 2022, 92.6 percent of deaths are among people above 65 years old.
Statistics reveal over 800,000 deaths among people ages 65 and older since the pandemic began, accounting for 75 percent of all COVID deaths to date.
A study conducted on the older population suggests the severity and outcome of COVID-19 largely depend on a patient’s age. Adults 65 years of age and older represent 80 percent of all hospitalizations, and have a greater risk of death than people under the age of 65.
Researchers believe that age-related decline and weakening of immune function are key factors contributing to the heightened vulnerability to severe COVID-19 outcomes in older adults.
Of the deaths observed in older populations, the majority were witnessed in patients with pre-existing conditions and comorbidities. Alongside the natural progression of aging, older adults are also more likely to have one or more serious underlying or known chronic conditions that put them at higher risk. These conditions might include diabetes, a heart condition, chronic lung disease, liver disease, and chronic kidney disease.
How Does Age Impact Immunity?
The immune system is made up of various organs, proteins, and cells. It protects the body from harmful pathogens, germs, and cell changes that can make us sick. When our immune system stops working appropriately, because it’s weak or can’t fight aggressive germs, we become ill.
The immune system’s functions begin to decline as we age. The most significant changes have to do with stem cells and T cells.
All immune cells come from stem cells. Adult stem cells generate replacements for the immune cells that are lost due to illness, injury, or disease.
When we age, our stem cells decrease and there becomes a reduction in their ability to regenerate cells. When this occurs, the number of our immune cells also decreases, which impacts our ability to fight infections.
Once the stem cells decline, the T cell population also decreases. T cells are important immune cells responsible for killing infected cells. When T cells reduce and their function becomes impaired, the infected cells cannot be killed and then a virus can spread to other cells and tissues.
A 2009 review indicated the age-associated decline of the immune system is characterized by extreme changes in T cell function.
Researchers note that the impact of aging on specific T cells has been tough to examine, but recent advances have provided new insights into T cell function and have allowed for a more precise examination of how T cells respond to aging.
Studies have revealed that age-related enhancement of Th17 (a helper T cell) generation and regulatory T cell function may contribute to substantial changes in immune function that can affect the immune response to infections, vaccinations, and tumors.
How to Fight Against Immunity Aging
Healthy eating habits and physical fitness can help nourish the immune system and keep it functioning well as we age.
Healthy Diets
Eating adequate nutrients as part of a diverse diet is required for the strength and function of all cells, including immune cells.
Examples of nutrients that have been identified as critical for the growth and function of immune cells include vitamin C, vitamin D, zinc, selenium, iron, and protein. These nutrients are found in a variety of animal and plant foods.
The stomach is a major site of immune activity and the production of antimicrobial proteins. Diet plays a key role in determining what kinds of microbes live in our intestines. A high-fiber, plant-rich diet with plenty of whole grains, fruits, vegetables, and legumes appears to support the growth and maintenance of beneficial microbes.
Microbes break the fibers down into short-chain fatty acids, which have been revealed to stimulate immune cell activity. These fibers are also called prebiotics.
Diets containing probiotic and prebiotic foods may boost immune function. Probiotic foods include live helpful bacteria whereas prebiotic foods contain fiber and oligosaccharides that feed and sustain healthy colonies of those bacteria.
A 2021 study revealed that eating a healthy diet is associated with a reduced risk of developing COVID-19 and its severe complications. Scientists found that people who reported eating the most fruits, legumes, and vegetables had a 9 percent lower risk of getting COVID and a 41 percent lower probability of developing severe COVID when compared with people who reported eating the least volume of fruits and vegetables.
The study’s lead author noted that the researchers think nearly a third of the COVID-19 cases could have been prevented if poor diet or socioeconomic disadvantages could have been removed.
Physical Activity and Exercise
A study suggests that a regular and age-appropriate exercise program can help older adults to lead a quality life by increasing cell count and preserving immune function.
Research reveals aerobic exercise may reverse the effects of aging in stem cells by increasing the amount of protein cyclin D1. Exercise returns cyclin D1 in dormant stem cells back to youth levels, effectively accelerating muscle stem cell generation.
Scientists believe that endurance exercise later in life is associated with a lesser age-related decline in certain aspects of T cell function. It’s believed moderate exercise should help reverse the adverse effects of aging by increasing the production of endocrine hormones.
A study suggests that routine physical activity may help protect people who get COVID-19 from becoming critically ill.
Serious health issues that are linked to the lack of exercise, such as obesity, heart disease, and diabetes, have also been associated with a greater risk of severe illness and death from COVID-19.
In this study, researchers analyzed data from more than 48,000 adults over the age of 18 who had confirmed COVID-19 diagnoses between January and October 2022. The group was divided into three categories:
- Consistently exercised for over 150 minutes per week
- Consistently inactive with only 0–10 minutes per week
- Active between 11–49 minutes per week, or who had variability in their exercise patterns
Scientists also investigated other important characteristics such as age, sex, race, body mass index, and smoking status. They looked at chronic conditions such as high blood pressure, cardiovascular disease, diabetes, and kidney disease, trying to identify if these patients were immunocompromised for any reason.
Findings revealed that people who were consistently inactive had a significantly higher risk of hospitalization and death after getting COVID-19 than those who were active for at least 150 minutes per week.
While those who were active for over 10 minutes per week had some shield against severe illness or death from COVID-19, they didn’t have as much protection as those who exercised for 150 minutes.
References:
Mueller AL, McNamara MS, Sinclair DA. Why does COVID-19 disproportionately affect older people? Aging (Albany NY). 2020 May 29;12(10):9959-9981. doi: 10.18632/aging.103344. Epub 2020 May 29. PMID: 32470948; PMCID: PMC7288963.
Centers For Disease Control and Prevention. Provisional COVID-19 Deaths by Week, Sex, and Age. www.data.cdc.gov/NCHS/Provisional-COVID-19-Deaths-by-Week-Sex-and-Age/vsak-wrfu/data Web. Assessed November 30, 2022
Centers for Disease Control and Prevention. Understanding Risk. www.cdc.gov/coronavirus/2019-ncov/your-health/understanding-risk.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fneed-extra-precautions%2Findex.html Web. Assessed November 30, 2022.
Lebrasseur A, Fortin-Bédard N, Lettre J, Raymond E, Bussières EL, Lapierre N, Faieta J, Vincent C, Duchesne L, Ouellet MC, Gagnon E, Tourigny A, Lamontagne MÈ, Routhier F. Impact of the COVID-19 Pandemic on Older Adults: Rapid Review. JMIR Aging. 2021 Apr 12;4(2):e26474. doi: 10.2196/26474. PMID: 33720839; PMCID: PMC8043147.
Administration for Community Living. COVID-19 Response. www.acl.gov/COVID-19 Web. Assessed November 30, 2022.
Mayo Clinic. Stem Cells: What are they and what do they do? www.mayoclinic.org/tests-procedures/bone-marrow-transplant/in-depth/stem-cells/art-20048117 Web. Assessed November 30, 2022.
National Institute of Health. Healthy Aging Tips for Older Adults in Your Life. www.nia.nih.gov/health/healthy-aging-tips-older-adults-in-your-life Web. Assessed November 30, 2022.
Barlow P, Reeves A, McKee M, Galea G, Stuckler D. Unhealthy diets, obesity and time discounting: a systematic literature review and network analysis. Obes Rev. 2016 Sep;17(9):810-9. doi: 10.1111/obr.12431. Epub 2016 Jun 3. PMID: 27256685; PMCID: PMC4988386.
Chen Y, Klein SL, Garibaldi BT, Li H, Wu C, Osevala NM, Li T, Margolick JB, Pawelec G, Leng SX. Aging in COVID-19: Vulnerability, immunity and intervention. Ageing Res Rev. 2021 Jan;65:101205. doi: 10.1016/j.arr.2020.101205. Epub 2020 Oct 31. PMID: 33137510; PMCID: PMC7604159.
Moffat SD, An Y, Resnick SM, Diamond MP, Ferrucci L. Longitudinal Change in Cortisol Levels Across the Adult Life Span. J Gerontol A Biol Sci Med Sci. 2020 Jan 20;75(2):394-400. doi: 10.1093/gerona/gly279. PMID: 31714574; PMCID: PMC7176109.
Bajaj V, Gadi N, Spihlman AP, Wu SC, Choi CH, Moulton VR. Aging, Immunity, and COVID-19: How Age Influences the Host Immune Response to Coronavirus Infections? Front Physiol. 2021 Jan 12;11:571416. doi: 10.3389/fphys.2020.571416. PMID: 33510644; PMCID: PMC7835928.
Venjatraman JT, Fernandes G. Exercise, immunity and aging. Aging (Milano). 1997 Feb-Apr;9(1-2):42-56. doi: 10.1007/BF03340127. PMID: 9177585.
" Conservative News Daily does not always share or support the views and opinions expressed here; they are just those of the writer."




Now loading...